On August 31st, a research team from the School of Life Sciences of ECNU published an online article entitled “Non-viral, specifically targeted CAR-T cells achieve high safety and efficacy in B-NHL” in Nature, a leading international scientific journal. This is the first study to report the development of a new generation of non-viral specifically integrated CAR-T cell technology and its effectiveness in a clinical trial for the treatment of relapsed and refractory non-Hodgkin's lymphoma.
This original study was a collaboration among the team of Zhang Jiqin, Liu Mingyao, Du Bing and Li Dali from the School of Life Sciences, ECNU, the team of Huang He and Hu Yongxian from the First Affiliated Hospital, School of Medicine, Zhejiang University and BRL Medicine Inc.
Victoria Aranda, a Senior Editor of Nature, commented that “This study provides a thoughtful pre-clinical framework for the design and implementation of a therapy using non-viral, targeted CAR-T cells. The authors provide promising early clinical results on the safety and the potential efficacy of this treatment in B-NHL.”
One of the reviewers, Professor Justin Eyquem of the University of California, commented that “This study reports the first clinical trial using CAR-T cells in which PD-1 is disrupted by integrating a CAR encoding gene into its sequence. The high complete-remission rate with low associated toxicities is an exciting outcome and suggests that the CAR-T cells are potent and safe. The authors also show the feasibility of using non-viral, gene-specific targeting in T cells for clinical application. This method will pave the way to more gene-targeted CAR-T-cell therapies, providing an important step for the field.”
This study reports the first clinical trial of PD1 downregulation targeted integrated CAR-T cells. The researchers observed a high rate of complete tumor remission without serious adverse events in the clinical treatment. The surprising result demonstrates the high clinical safety and efficacy of CAR-T cell therapy, and its feasibility in clinical application. This technological innovation lays a solid foundation for the future development of genetically targeted modified CAR-T cell therapy and is an important boost to the development of the field.
“The previous method of tumor treatment was to use drugs to kill tumor cells. More and more studies in recent years have found that it is possible to kill tumors by enhancing the function of immune cells, and that this treatment may bring about great efficacy. From my perspective, this is an exciting research direction,” said Associate Professor Zhang Jiqin, first author and co-corresponding author of the article.
First and co-corresponding author Zhang Jiqin
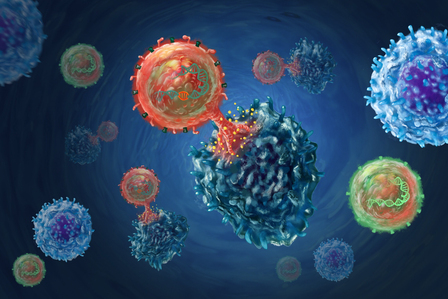
CAR-T (Chimeric antigen receptor T, CAR-T) cell therapy, which is globally popular in recent years, is one of such immune cell therapies. Unlike traditional anti-cancer drugs, CAR-T cell therapy is a treatment that isolates T lymphocytes from patients’ bodies, “transforms them artificially” in vitro and infuses them back into patients’ bodies to kill cancer cells.
However, globally, much technological improvement is required for CAR-T therapy, especially the preparation method. Currently, CAR-T cells are mainly prepared by viral infection, of which the drawbacks include high production cost, long preparation time, complicated process and potential tumorigenesis risk.
“To overcome these drawbacks, we have developed a new technical approach and demonstrated that this next-generation CAR-T technology is safe and effective by a clinical trial,” said Zhang Jiqin.
Through extensive exploration of conditions and method optimization, the research team successfully achieved efficient integration of CAR sequences at genome-specific sites with CRISPR/Cas9 gene editing technology. After demonstrating the feasibility of the technology through in vitro and in vivo tumor killing tests, the team further prepared anti-CD19 non-viral PD1 integrated CAR-T cells (PD1-19bbz) and finally applied it to the clinical treatment of relapsed and refractory non-Hodgkin’s lymphoma.
In the eight treated patients, researchers observed high clinical safety and efficacy of PD1-19bbz. Complete remission of disease was achieved in 87.5% (7/8) of patients, and five of them have experienced cancer-free survival exceeding one year.
“We treated patients who could not be cured by conventional chemotherapy and radiotherapy or had relapses after treatment, and this clinical result proves that all the effort of these five and a half years was worthwhile,” said Zhang Jiqin.
From left: Du Bing, Zhang Jiqin, Liu Mingyao, Li Dali
Link to the paper: https://www.nature.com/articles/s41586-022-05140-y
Source: School of Life Sciences
Editor: Cui Jizhen